The Long COVID Rundown, Sept 2024
This month, Long COVID led me to vaccines, an operating room, and the NIH
1. I got vaccinated: Which vaccine will you choose?
Novovax vs mRNA has been a trending topic in the Long COVID social media space. Why?
Novavax is designed differently than the mRNA-based vaccines made by Pfizer and Moderna. It’s become a popularized option for patients with Long COVID, with some people choosing to remain unvaccinated (or unboosted) until and unless they can received Novavax. I’ve read accounts of individuals traveling from Canada to the US for the vaccine before Novavax became available in the Canadian medical system. Someone on X claimed that, because his insurance company only covered Pfizer and Moderna vaccines, he and his wife chose to pay a hefty sum for Novavax. These types of stories are rarely verifiable, but they receive tremendous engagement and support. The sentiment, as I interpret it, is that insisting on Novavax is a form of self-advocacy. It’s perceived as a way to keep yourself safe.
What makes Novavax different and attractive? Is it safer? Unsurprisingly, the answer is ‘maybe’.
Novavax Mechanism May Be Safer for Long COVID
The mechanism that protects us from severe infection is ultimately the same for all COVID vaccines. As Kathy Katella explained for Yale News: “Cells in the body recognize that a spike protein (the spikes you see sticking out of the coronavirus in pictures) doesn’t belong, and the immune system reacts by activating immune cells and producing antibodies to attack the real virus if you get exposed.”
To trigger that immune response, mRNA-based vaccines made by Pfizer and Moderna include viral particles from the COVID spike protein itself. Novavax uses a lab-created version of the spike protein that does not have genetic material from the virus and cannot cause disease. This version of spike protein is in the form of a nanoparticle, and it’s delivered with an adjuvant. An adjuvant is an ingredient that helps the immune system recognize that nanoparticle and stimulate the needed immune response. That’s why you’ll see Novavax officially listed as “Novavax COVID-19 Vaccine, Adjuvanted (2024-2025 Formula).” Novavax gave their proprietary adjuvant a name with leather trench coat vibes: Matrix-M.
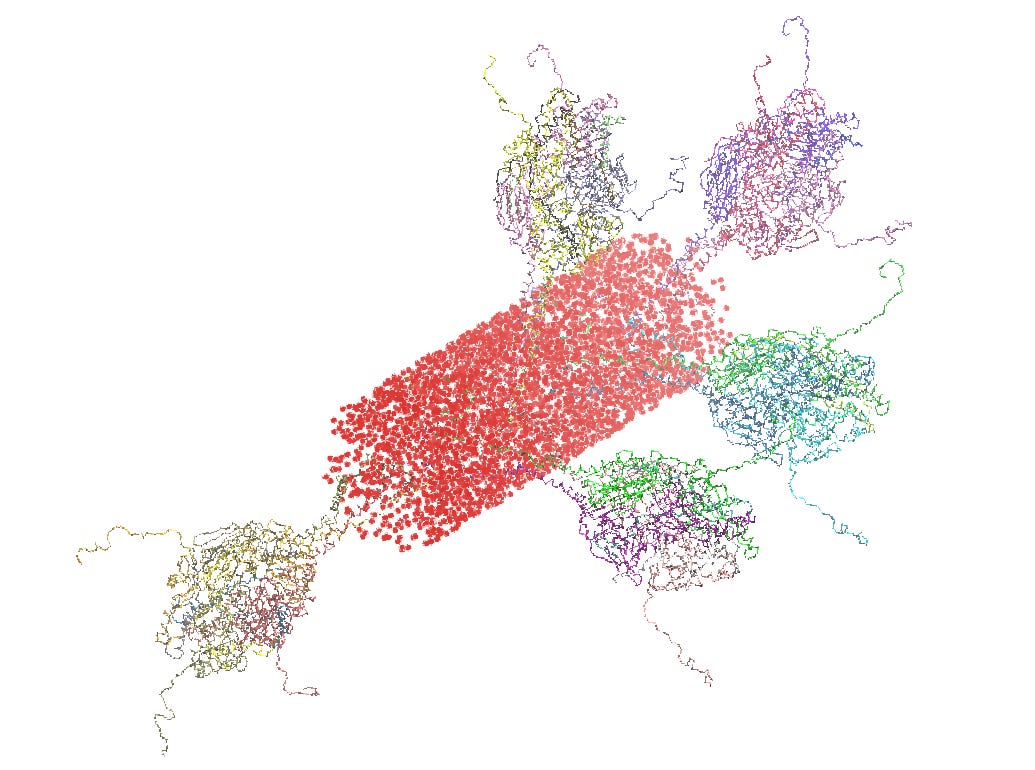
Among people with Long COVID, Novavax has been attractive for its lack of genetic viral material. There is a theory that our Long COVID symptoms are caused by circulating virus that doesn’t clear the body. This theory, called ‘viral persistence,’ is a major focus of Long COVID research. If viral persistence is substantiated, we would still need to establish the extent to which spike protein is involved. If spike protein does trigger Long COVID, it makes sense to avoid any exposure to it, whether by infection or vaccine. A Harvard study demonstrated that in patients with Long COVID, spike protein continues to circulate for up to a year. That being said, some participants who did not have Long COVID also showed prolonged spike protein in their blood.
For some, Novavax is preferable for another reason: it has a milder side effect profile. Patients report less myalgia, fatigue, pain and fever after injection. For people with Long COVID, who are often debilitated by these types of symptoms already, avoiding a crash from vaccination is a priority.
Is Novavax as effective against COVID-19 as mRNA vaccines?
To answer this question, let’s talk about how and why vaccines are updated. And let’s talk about target strains.
Vaccines are updated to match the most commonly circulating strains of virus. This happens for the flu vaccine every year. The Centers for Disease Control (CDC), in consultation with the World Health Organization, predicts flu strains that will most likely circulate in the upcoming flu season. The US Food and Drug Administration (FDA) then makes the final decision on the viruses to target in the annual vaccine, at least in America. This prediction takes tremendous effort, and is based on data collected by epidemiologists and infectious disease professionals. It has to be a prediction made in advance, because it takes time to produce targeted vaccines. Ideally, the CDC predicts the exact strain that will become dominant, but that’s very hard to do. Typically, the flu vaccine targets a strain that is similar enough to the dominant strain that it yields benefit. This recurring act of collecting data, pinpointing variants, manufacturing and distributing life-saving vaccines every year is, in my view, nearly miraculous. It is a powerful example of the way a bureaucracy is actually used to benefit the masses.
The process of updating COVID vaccines follows a similar practice, and the CDC identified the Omicron JN.1 lineage as the target. The 2024-2025 mRNA and Novovax COVID vaccines both target the lineage, but different viral strains. Pfizer and Moderna’s vaccine targets the KP.2 strain, which is a mutation of JN.1 and was the dominant circulating variant earlier this year. Novovax targets JN.1, which is currently less common. Luckily, the strains are similar enough that a JN.1 vaccine will offer protection against a KP.2 infection.
The thing is, neither of these are currently the most dominant strain. That honor is now held by KP.3. KP.3 is also related to JN.1, so we expect all current vaccines to offer protection. But we know KP.3 won’t be the dominant strain forever. COVID-19 is a quickly mutating virus which will require regularly updated vaccines. One reason is that the immunity we develop after infection or vaccination wanes. Data suggests protection against severe infection from mRNA vaccine can last 6 months, versus 4 months for Novovax (please note there is much more nuance to this than my statement captures). Furthermore, as the virus mutates, the anti-COVID antibodies we do retain may not be specific enough to fight a new strain.
It’s important to note here that, because of the differences in their technology, mRNA vaccines can be updated more quickly than protein-based vaccines like Novavax. In order for Novavax to remain a viable option going forward, the process of predicting strains will be even more important. Either that, or Novavax develops a way to more quickly update their vaccine. An ideal option, of course, is a vaccine that provides us immunity regardless of mutation. That’s not yet available.
Additional Novavax considerations
Efficacy: Like the mRNA-vaccines, Novavax effectively prevents severe COVID infection and hospitalization, particularly for high-risk patients. It performed slightly less effectively than mRNA vaccines at preventing symptoms from a COVID-19 infection for lower-risk groups. Neither vaccine is very effective at preventing transmission. Much greater benefit lies in reducing symptom severity, reducing hospitalization and death from COVID-19.
Long COVID: Vaccination likely reduces risk of developing Long COVID. How vaccination affects existing Long COVID symptoms has yet to be studied sufficiently. How mRNA compare to Novavax in this regard is not established.
Allergy*: Both Pfizer-BioNTech and Moderna mRNA-based vaccines use polyethylene glycol (PEG) as a stabilizer, and in some people this can cause an allergic reaction. Novavax does not contain PEG but does contain a nother possible allergen called polysorbate.
Myocarditis remains a risk for both types of vaccines. It typically develops about 10 days after vaccination. Adolescent boys and young men are at greatest risk.
Pregnancy: Novavax has not been studied as well as Pfizer and Moderna in pregnant and/or breastfeeding individuals. Consult with your obstetrician
Children: Novavax is approved for use in people 12 years of age and older. mRNA vaccines can be administered to children under 12, including infants.
I received the updated Novavax vaccine. I chose it primarily because of its milder side effect profile, although I do wish it targeted KP.2. I felt tired for a few days after and had a slightly sore arm. I developed a migraine headache the day after. Whether the headache can be attributed to the vaccine, I don’t know. Recurrent headaches have been a problem for me since falling ill in 2020. Regardless, my symptoms after Novavax are much milder than symptoms after the mRNA vaccines I’ve received.
Here is CDC guidance on updated vaccination against COVID-19.
*This section has been updated for accuracy and now contains links to reference.
2. I survived anesthesia and held a Q&A about it.

Consequences of my Colonoscopy
Earlier this month I underwent colonoscopy for cancer screening. I celebrated my 45th birthday a few months ago and decided to follow American Cancer Association recommendations to begin screening for colorectal cancer. While there are less invasive methods of screening, including a test like ColoGuard that can be done at home, colonoscopy is the only screening method that allows a physician to not only screen for cancer but remove questionable growths at the same time. The primary reason I chose colonoscopy, however, is that I also planned to have an upper endoscopy to help evaluate my chronic abdominal pain. Both require anesthesia and can be done in the same visit. A gastroenterologist, also called a GI doctor, inserts a camera into the mouth to evaluate the esophagus and stomach - that’s called an upper endoscopy. They use a different type of camera in the back end to examine the rectum and colon. I have provided anesthesia for many cases like this, and knew I would be comfortable under sedation administered by an anesthesiologist.
Before a colonoscopy, the rectum and lower colon need to be clear of stool. So, following my doctors’ instructions, I changed my diet in the days leading up to the procedure. Starting the day before my procedure, I stopped eating solids and drank only clear liquids. I also used a very effective prescription laxative. I wasn’t bothered by hunger and the taste of the laxative wasn’t the worst, but I did become dehydrated. The morning of the procedure, I became slightly dizzy, and since my stool was clear I stopped drinking any more of the laxative. By the time I made it to the pre-op gurney, I was dehydrated enough that my veins were very hard to find. My anesthesiologist ultimately used an ultrasound machine to place an IV in a small vein.
Bowel prep runs the risk of dehydration for anyone, but dehydration can have significant consequences for people with Long COVID. It can worsen POTS-type symptoms, trigger headaches and post-exertional malaise. If you require a colonoscopy, be sure to discuss your Long COVID symptoms with your doctor and, as always, listen to the signals your body sends you. When I felt dizzy, I knew I had reached my limit. Whatever level of bowel prep I had completed was the best I could do. Fortunately, as my recovery nurse told me, I was “plenty cleared out.”
Don’t hesitate to ask your doctor for modifications in bowel prep, as there are many options. Ask to be scheduled at a time of day that works best for you, remembering that you will have to wake up several hours before the procedure to complete your bowel prep, and that you will remain in the post-op care unit at least 30 minutes to an hour after the procedure. Have a reliable ride home, and have a plan for recovery. Clear your schedule for a few days after. Ask your anesthesiologist to generously administer IV fluids, safely of course, to offset the toll of dehydration. Stay in the recovery room until you are clear-headed and not light-headed.
Anesthesia and Long COVID
Inspired by the procedure, I held a Q&A last week answering your questions about anesthesia and Long COVID. The most pressing concern people have is how to prevent catching COVID in the hospital. People posed many questions about the dentist, too. Undergoing anesthesia makes us feel vulnerable, and when we don’t fully trust our care team, we’re right to be afraid. I strongly urge you to keep up to date on preventive care measures, including dental visits, mammograms and colon cancer screenings (you don’t always require a colonoscopy), to catch medical issue early. Remember, small problems require small interventions, and may prevent the need for surgery. Small interventions are not without risk, but the odds are much better than letting the issue fester.
Find more answers to listener questions in the most recent podcast episode. You can also read advice I give anesthesiologists providing care for Long COVID patients.
3. RECOVER-TLC: What is the future of Long COVID research?
Twitter was actually fun last week, because the Long COVID community collectively participated in the RECOVER-TLC meeting. The three-day meeting was held in person and made available as a webinar. Hosted by the National Institute of Allergy and Infectious Disease (NIAID), it focused on the future of Long COVID research. As a community, we live-tweeted panel meetings, hyped up our friends and colleagues before their presentations, and shared our thoughts in real-time. Since this disease by its nature isolates us, this communal experience has been very meaningful to me.
A lot of my feed looked like this, and the conversations continue. The theme in the patient community has been collaboration. Many posts share info, tag and amplify others.
As I explain in podcast Episode #9, RECOVER is the federal initiative dedicated to Long COVID research. So far, the National Institutes of Health have allotted over one billion dollars to Long COVID research, yet we have identified no reliable treatments. RECOVER has been criticized for investing very little money in clinical research, and for funding initiatives like cognitive behavioral therapy and neuro-psychological coping skills, instead of medications.
While continued funding for Long COVID is tenuous, RECOVER still has hundreds of millions of dollars earmarked for research. The recent conference, RECOVER-Treat Long COVID (TLC) was meant to explore ways the remaining funds will be used, by fostering collaboration between researchers and patient advocates.
I am dedicating a future podcast episode to RECOVER-TLC but I will note some highlights. FDA policy analyst Heather Stone’s presentation on the CURE-ID database was impressive. She explained the need to identify medications that could be repurposed for Long COVID. Patient testimonies and messages of urgency from researchers were also very powerful. Here are a few that left an impression on me.
Panelists and Patients at RECOVER-TLC
“You look fine on the outside, but on the inside, nothing works.”
“What would happen if Long COVID was declared a public health emergency?”
“What is ‘recovered’?”
“Nobody with [post-exertional malaise] lives a normal life.”
“You are the NIH. You are the leaders.”
I’ll dive in more to RECOVER-TLC on the pod and newsletter soon.
4. This Substack Grew! Welcome!
My kids are in a growth spurt. Some mornings they walk downstairs and I swear their pajamas are shorter. I have to do a double-take. I’ve got the same whiplash here on Substack. Long Covid, MD has grown very quickly this month. Thank you for subscribing.
As I wrote on a recent Note, the speed at which Long Covid, MD is growing reflects a need for medical care that millions simply cannot access. I’ve used Substack’s resources to learn how to use this platform, how to build my site, and how people measure success here. I’ve hit metrics in 30 days that others work to gain over years. Is that good? Or is that sad? I think it’s both, and I think it simply reflects a need. My hope is that someday soon we don’t need Long Covid, MD, because answers to our chronic illness will be easy to find.
For now, I’m here. My Substack inbox is open, as is my email. Let me know how I can use this platform to help, or just say hi. I hope you’re feeling well. Bye for now!
Where did Long COVID lead you this month? Did we land in any of the same places?





Great post, doc - thank you. You have a knack for explaining things quite clearly.
I haven’t gotten a C-19 vaccine since 2021. My functional medicine doctor last year said he could not in good faith advise any of his several long COVID patients to get one, since “we just don’t know enough about what is going on with your immune systems and what these vaccines might be doing to you.” I’ve just been taking other precautions. Fortunately I’ve only had the March 2020 infection. A good friend who is also a long hauler opted for Novavax in late 2023 and had a really terrible flare of symptoms that included new onset POTS. She previously didn’t react at all to several mRNA shots. So strange.
Thank you for this helpful article - and especially for tackling the difficulties we face with bowel preps. Finding an understanding doctor who will work to make the prep safe is SO important.